

Andropause and Men
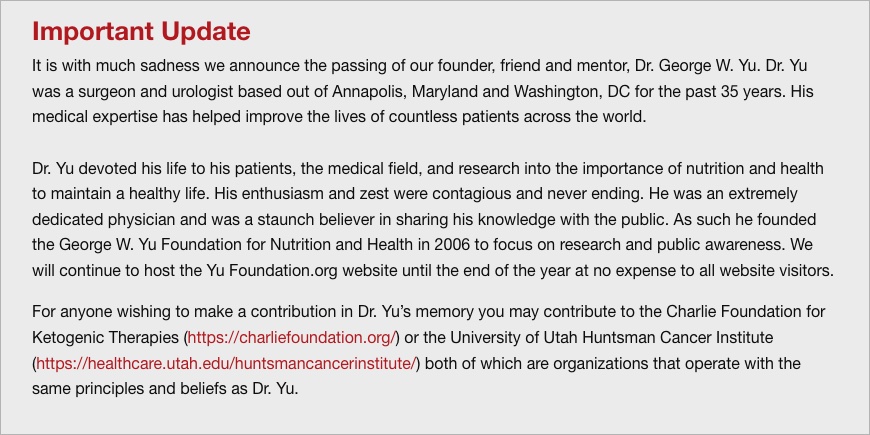
Andropause - Decline in testosterone secretion by testicular Leydig cells in aging men, ADAM Androgen Decline in Aging Men, Hypogonadism with Aging
All the above terms mean the same- a gradual decline in men’s hormone balance.
Background of My Interest
What I witnessed in 1978 at Johns Hopkins Hospital, working with W.W. Scott on the NCPC project and his private patients, have had a lasting impression on my career. We cared for 100 men with advanced prostate cancer who went into rapid "Andropause" with surgical or chemical castration.
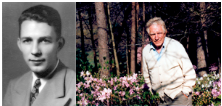
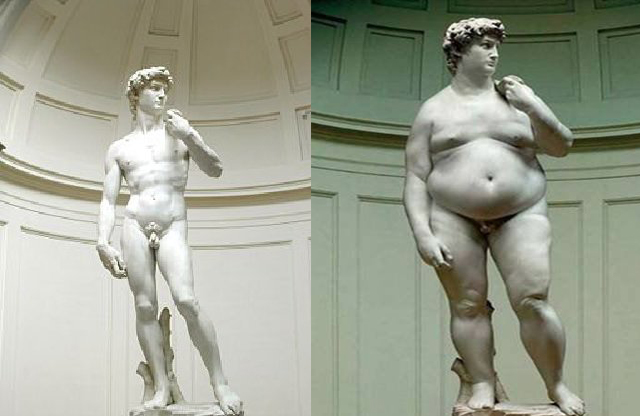
They all abruptly had "hot flashes" with immediate severe fatigue with loss of erectile function, lost muscle in exchange for a fat belly, lost bone mass, became anemic with fatigue, many developed insulin resistance with abnormal glucose tolerance tests and became overt Diabetics within one 1 year period.
But most of all, they were alive for the period of five 5 years but “lost interest in life and stopped what they loved to do.
Natural History of Hormonal Decline
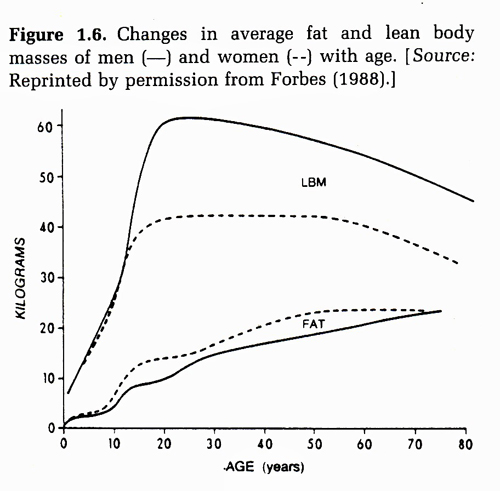
In a one year period I saw a "fast movie forward" of what happens to aging men after age 35 on.
From age 35 on, there is a 2% decline in testosterone every year and therefore it is a "slow motion movie" of what I witnessed. Testosterone hormone decline is not always correlated with lower sperm production and elderly men can continue to produce sperm counts up to 200,000,000s /per ejaculate with decreasing numbers and quality over time.
This natural change occurs over a 40 to 50 year period without the profound symptoms of “Hot Flashes” seen in women and castrated men. Contrasted to women going through Menopause which is a more abrupt end of the cyclical high hormone elevations, Andropause is slower, subtle, but real!- and labeled as just “Aging Men”. What I witnessed is a form of abrupt andropause induced by castration for advanced prostate cancer represents a scientific “human model” of metabolic and medical changes in men as a consequence of testosterone depletion.

Research Supporting My Impression in 1978
14 years later, 1992-1993 Marin, Holmang and Bjorntorp of Sweden confirmed that it was testosterone (not dihydrotesterone) that regulated glucose metabolism leading to “Insulin Resistance” in castrated animal models and showed immediate reversal by replacing testosterone within 48 hours- thus a “nongenomic effect”. They also confirmed the reversal effect on abdominally obese men by testosterone treatment could attenuate their abnormal glucose and insulin profile and make them appear “younger and healthier.”
By 1998, Mauras and Veldhuis showed that young healthy men chemically castrated can become and appear “older” by loss of muscles and strength, increase in fat deposits in all subjects studied. All findings reversed when the temporary castration effect was gone and the subjects returned to their younger state and appearance again.
By 2005, 2007, and 2008, Pittleloud, Hayes, Yialamas, and Baseria of USA all confirmed human clinical evidence that castration led to a metabolic dysfunction with insulin resistance and Diabetes. The title “Androgen deprivation therapy, insulin resistance, and cardiovascular mortality: An inconvenient truth-Baseria” pointed that castration as treatment for advanced prostate cancers has huge metabolic consequences. Pittleloud speculated that testosterone depletion may lead to a mitochondrial subcellular dysfunction which may lead to a worse consequence than the temporary benefits of castration in men with metastatic prostate cancer.
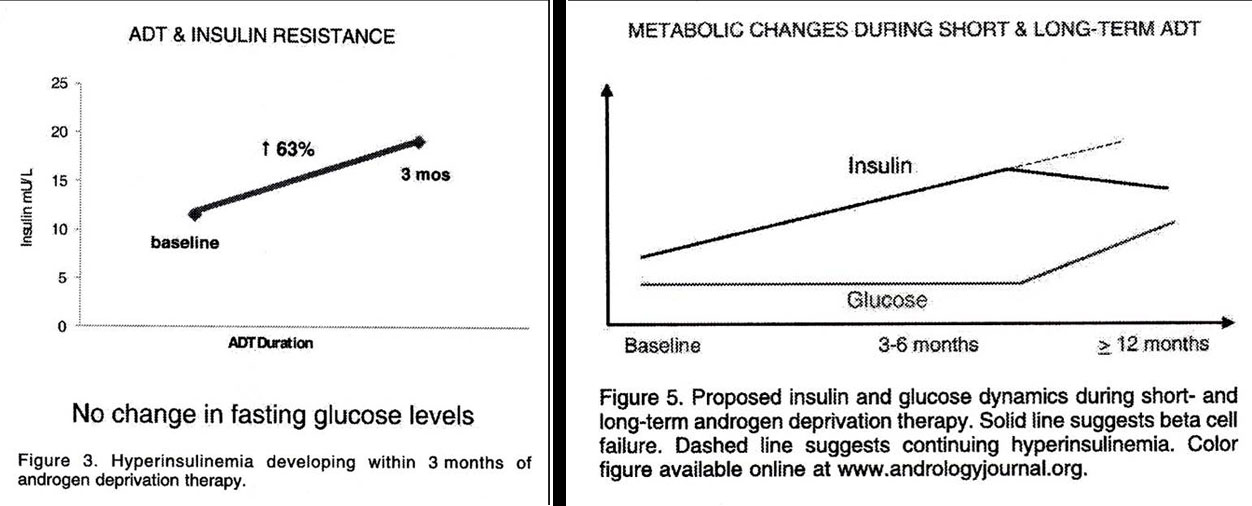
In 2011, Triash and Yu, proposed that castration leading to symptoms of hot flashes, severe fatigue, erectile dysfunction, insulin resistance, and finally clinical diabetes is a spectrum of increasing “Mitochondrial dysfunction” at the cellular level which can lead to further medical problems. Since castration does not cure advanced prostate cancer, should doctors chemically castrate them for a temporary benefit and put them at risk for other medical diseases?
Intermittent Androgen Deprivation (IAD)
Proponents of total and aggressive androgen deprivation call the subsequent symptoms and signs as slight decline in the “Quality of Life” but I believe it is a major disruption of life itself with all kinds of medical consequences such as diabetes and cardiovascular disease.
Growing numbers of urological surgeons resort to chemical or surgical castration only as a last resort for aggressive metastatic prostate cancer disease and use an intermittent androgen deprivation (IAD) instead of a total deprivation as the metabolic consequences noted above are just as bad as the disease, their prostate cancers! European and Canadian studies show that whether intermittent or total castration, the patient survival is the same with terminal death at the endpoint. I personally have witnessed and cared for some medical doctors using IAD for as long as 15 years.
For the near future, we must emphasize prevention of prostate cancer and consider other forms of therapy other than more androgen deprivation for progressive prostate cancer! Even from 1950s on, W.W. Scott told me that every form of endocrine suppression has been tested but the bottom line is that it doesn’t cure the patient!
We must respect the value of maintaining men’s hormonal health as it has so many medical consequences and use IAD as needed and consider newer approaches to target prostate cancer metabolism (discussed in another section) and design newer chemotherapeutic agents and dosing with greater considerations of its slow doubling time (growth rate) of this unique cancer.
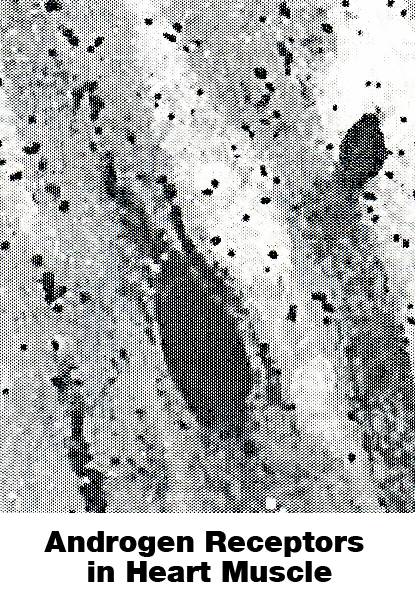
A Long-term View of Andropause
The use of hormonal deprivation as treatment for advanced prostate cancer has become a “human model” of how testosterone may influence many physiological and metabolic functions other than for reproduction. Clinically in aging, the Anabolic State of growth and repair is slowly replaced by the Catabolic State of atrophy and breath down- bone loss, all three types of muscle loss from skeletal (especially chest, arms and thigh), smooth involuntary muscles and cardiomyocytes of the heart occur, organ mass loss and anemia (lower red blood cell count) etc. with accumulation of the default tissues “fat” or adipose tissues. Triash (2005) showed that castrated animals developed fat infiltrate in the muscular smooth muscle compartment of the corporal cavernosa and reversed with testosterone replacement with abnormalities in the mitochondria.
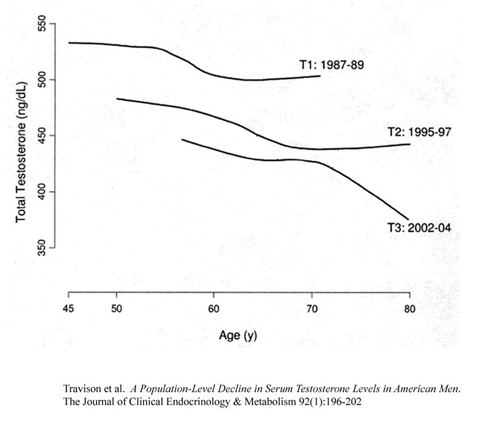
Travison and associates show that there is also a “Transgenerational” decline in testosterone levels. In other words your grandfather had more testosterone than your father and your father had more testosterone than you the same age set point. What is the cause?
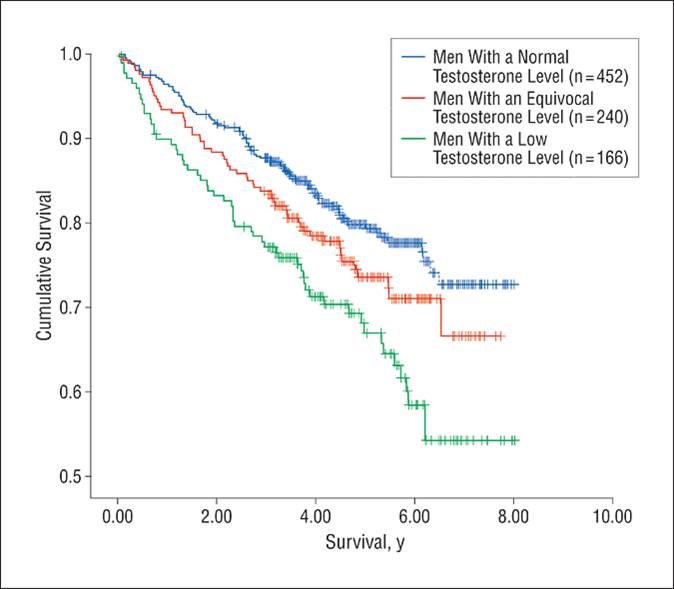
Shores (2006) showed that there is a higher mortality with lower testosterone levels. And recently, she showed that testosterone replacement improved survival (2012).
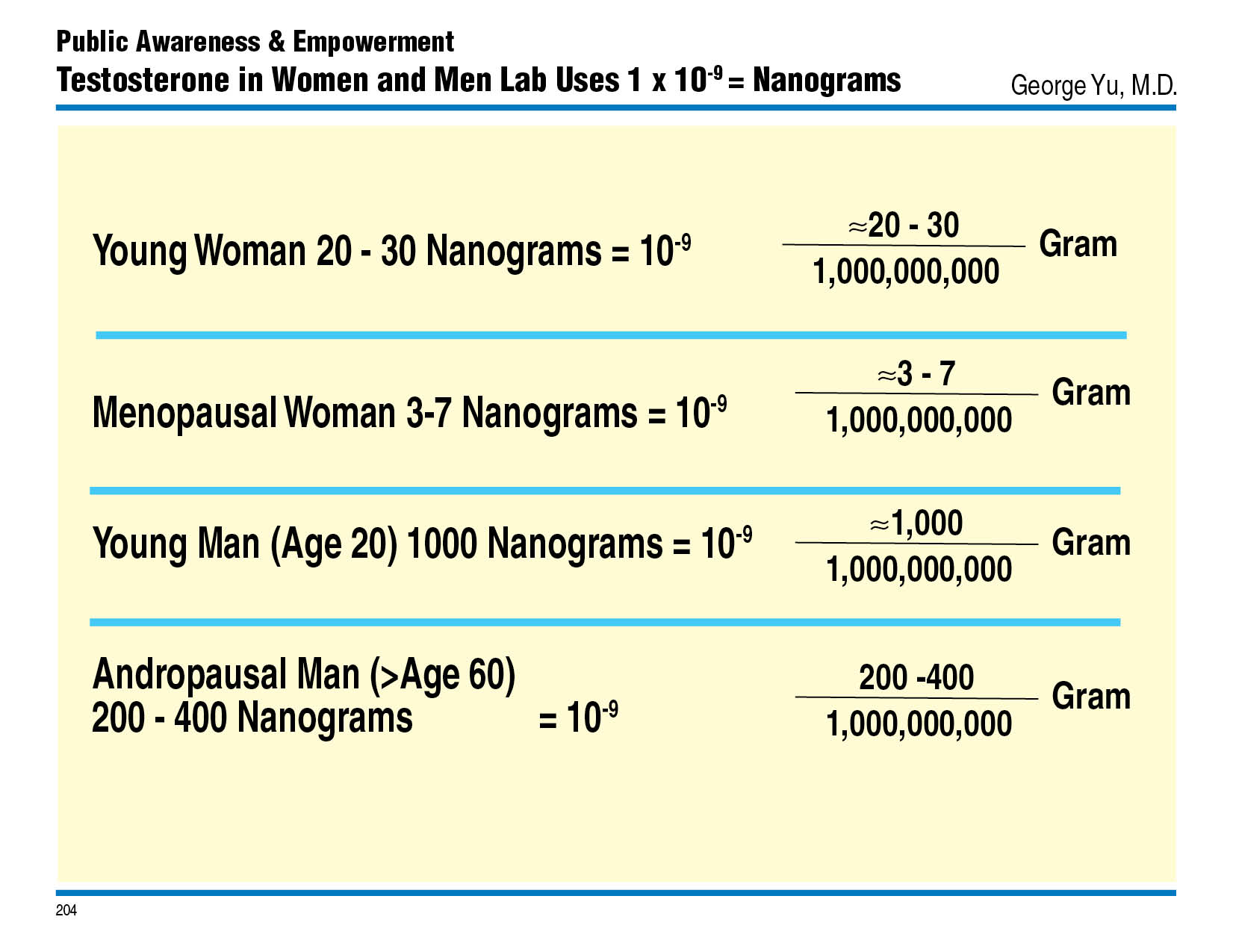
Testosterone Hormonal Baseline Comparison
The Hypothalamic-Pituitary-Endocrine Axis is Dynamic and Adaptive and Interacts with other hormones LH and FSH interacts with Testosterone, Estradiol Estrogen, Progesterone, Insulin Thyroid etc.
We now know that the hypothalamic-pituitary-gonadal axis is responsive and adaptive to the environmental milieu. It is probably true for all hypothalamic-pituitary-endocrine end- organ axis relationship. Looking only at Testosterone, we know that a man’s testosterone secretions will change not only with aging but with the following surrounding environmental changes:
- taking opioids medications
- have hypoxia from sleep apnea,
- in chronic adrenal stress situations
- work night shifts and changes regularly
- Seasonal changes
- an astronaut with changes in gravity
- have renal kidney failure
- have other chronic diseases such as lung disease or rheumatoid arthritis
- have Diabetes
- have metabolic syndrome
Testosterone response is "Adaptive" depending on your external and internal environment. Though we have guidelines for diagnosis of “hypogonadism” each person is different and “one shoe does not fit all”. Some men do well with low levels and some require more than the typical “Bell Curve” definitions of low, median, or higher than for age. Experience has taught me that management of patient is much more complex than giving a lecture giving a logical sequential answer! Also the importance of balancing hormones such as Testosterone and Estradiol and Estrone Estrogens plays a major role in man’s wellbeing. This holds even more profoundly in women, where the balancing of Progesterone to Estradiol is critical from youth to aging.
Testing Who You Are “Snapshot of your Hormone Movie”
You can get a baseline hormonal profile of yourself with venous blood, finger blood spot testing, urine testing and sometimes saliva testing. For men, Testosterone, free, total and bioavailable, Estradiol and Estrone estrogens, pituitary LH and FSH, pancreatic Insulin and hemoglobin A1c, Thyroid TSH with FreeT3 and FreeT4, growth hormone IGF-1, adrenal DHEA with Progesterone, and a cortisol saliva stress test to understand your biological age and hormone levels.